mucormycosis black fungus infection treatment hyderabad
India’s Covid-19 pandemic is getting much more complicated.
A devastating second wave of Covid-19, which sees the country registering around 350,000 new infections per day, has resulted in a massive increase in cases requiring powerful drugs. However, the long-term effects of these drugs lead to rare cases of fungal infection which can even prove to be fatal in some cases.
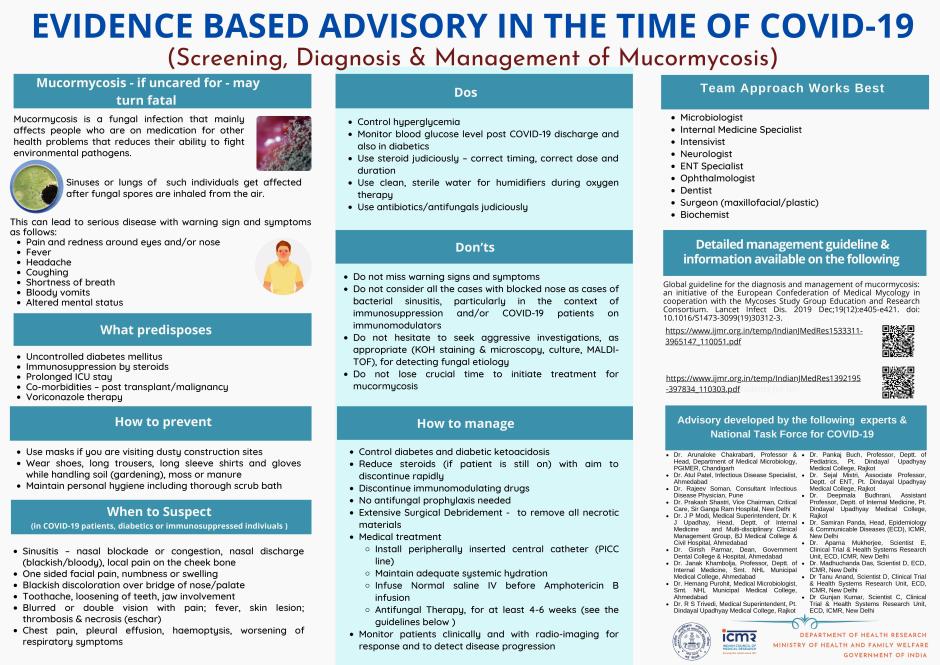
Mucormycosis, known as black fungus, is an infection that belongs to the group of mucormycete fungi. It is common in natural environments, especially in soil. Although rare, this infection has been around for decades, but only affects people with health problems and severely weakened immune systems due to steroid use.
Growing cases of mucormycosis in patients with Covid-19 are widespread, mainly due to the increased use of steroids such as dexamethasone, especially in diabetics. Not everyone is predisposed to black fungal disease, but the uncontrolled and unsupervised use of steroid therapy can often make things worse, even for safe patients.
Although it has not yet been classified as an epidemic, the Indian Council for Medical Research, the government’s main research body, has published a set of guidelines for the detection and treatment of mucormycosis.
If caught early, it is completely treatable.
Who is at risk of mucormycosis?
According to an infectious disease doctor at Hospitals in Hyderabad, there is a subset of people who are particularly susceptible to the disease. This includes patients with Covid-19 including:
Those who have received high doses of intravenous or oral steroids for long periods of time;
And those who have received immunomodulators (drugs used in diseases like cancer to change how the immune system responds)
Black Fungal Infection

Fungal Infection Overview
Mucormycosis is also know as Black Fungal Infection Treatment cost In Hyderabad a serious but rare fungal infection caused by a group of molds called mucormycetes. These molds live throughout the environment. Mucormycosis mainly affects people who have health problems or take medicines that lower the body’s ability to fight germs and sickness. It most commonly affects the sinuses or the lungs after inhaling fungal spores from the air. It can also occur on the skin after a cut, burn, or other type of skin injury.

What Causes Mucormycosis?
- Mucormycosis, also known as black fungus or zygomycosis, is caused by a group of mould called mucormycetes.
- These fungi live in the environment, particularly in soil and in decaying organic matter, such as leaves, compost piles, or rotten wood, according to the Center for Disease Control and Prevention.

Symptoms of Mucormycosis
Symptoms of rhinocerebral (sinus and brain) mucormycosis include:
- One-sided facial swelling
- Headache
- Nasal or sinus congestion
- Black lesions on nasal bridge or upper inside of mouth that quickly become more severe
- Fever
Symptoms of pulmonary (lung) mucormycosis include:
- Fever
- Cough
- Chest pain
- Shortness of breath

Dr. Amar Raghu

- MS (Gen Surgery), M.Ch (Plastic Surgery) (Varicose) Consultant
- Plastic & Cosmetic Surgery & Reconstruction Surgery
- 22+ Years Experience: Black Fungal Infection Treatment cost In Hyderabad
- Dr. Amar Raghu Narayan G is a Consultant Plastic & Cosmetic Surgeon at Continentals Hospitals. As a well trained surgeon, Dr. Amar Raghu has performed over 5000+ Major Surgeries in the fields of Hand Surgery involving finger reconstruction, tendon transfer, Acute Burnes and burn sequelae reconstruction, microsurgery involving replantation & Revascularisation, general plastic surgery, cleft lip and palate surgeries. He also specialises in Cosmetic Surgery involving rhinoplasty, liposuction, breast reconstruction, facial rejuvenation and contour corrections.
- During the course of his career, Dr. Amar Raghu has established a plastic surgery division, a Burns ICU and began an MCh Plastic Surgery Course under MCI guidelines. He is well published in national and international journals, and frequently attends Plastic & Cosmetic Surgery conferences around the world.
- Dr. Amar Raghu Narayan fluently speaks Telugu, English and Hindi.
★★★★★ 5 days ago
Reply Like
★★★★★ 7 days ago
Reply Like

People at Risk & Prevention Black Fungal Infection Treatment cost In Hyderabad
Who gets mucormycosis?
Mucormycosis is rare, but it’s more common among people who have health problems or take medicines that lower the body’s ability to fight germs and sickness. Certain groups of people are more likely to get mucormycosis, 1–3 including people with:
- Diabetes, especially with diabetic ketoacidosis
- Cancer
- Organ transplant
- Stem cell transplant
- Neutropenia pdf icon[PDF – 2 pages] (low number of white blood cells)
- Long-term corticosteroid use
- Injection drug use
- Too much iron in the body (iron overload or hemochromatosis)
- Skin injury due to surgery, burns, or wounds
- Prematurity and low birthweight (for neonatal gastrointestinal mucormycosis)

Is mucormycosis contagious?
No. Mucormycosis can’t spread between people or between people and animals.
And Today I’m going to show You the Imp
13 Exact Information about Black Fungal Infection Treatment cost In Hyderabad?

Where Mucormycosis Comes From

How is mucormycosis diagnosed?

★★★★★ 2 days ago
Reply Like

Treatment for Mucormycosis
How is mucormycosis treated?
IV bag for antifungal medicine, usually amphotericin B, posaconazole, or isavuconazole
Mucormycosis is a serious infection and needs to be treated with prescription antifungal medicine, usually amphotericin B, posaconazole, or isavuconazole. These medicines are given through a vein (amphotericin B, posaconazole, isavuconazole) or by mouth (posaconazole, isavuconazole). Other medicines, including fluconazole, voriconazole, and echinocandins, do not work against fungi that cause mucormycosis. Often, mucormycosis requires surgery to cut away the infected tissue
Types of mucormycosis
- Rhinocerebral (sinus and brain) mucormycosis is an infection in the sinuses that can spread to the brain. This form of mucormycosis is most common in people with uncontrolled diabetes and in people who have had a kidney transplant. 7-8
- Pulmonary (lung) mucormycosis is the most common type of mucormycosis in people with cancer and in people who have had an organ transplant or a stem cell transplant.
- Gastrointestinal mucormycosis is more common among young children than adults, especially premature and low birth weight infants less than 1 month of age, who have had antibiotics, surgery, or medications that lower the body’s ability to fight germs and sickness. 9-10
- Cutaneous (skin) mucormycosis: occurs after the fungi enter the body through a break in the skin (for example, after surgery, a burn, or other type of skin trauma). This is the most common form of mucormycosis among people who do not have weakened immune systems.
- Disseminated mucormycosis occurs when the infection spreads through the bloodstream to affect another part of the body. The infection most commonly affects the brain, but also can affect other organs such as the spleen, heart, and skin.
How can fungal infections be prevented?
Good hygiene is also critical for avoiding fungal infections.
Try to:
keep your skin clean and dry, particularly the folds of your skin
wash your hands often, especially after touching animals or other people
avoid using other people’s towels and other personal care products
wear shoes in locker rooms, community showers, and swimming pools
wipe gym equipment before and after using it
- 24×7 ICU
- Years of Experience21+
- 3500+ Liposuction cases
- cases 900+ Facial
- Affordable variocse veins treatment cost
- cosmetic surgery centreTop rated
- Board certified plastic surgeons
- Attached diagnostics
- Full Body Liposuction (One Sitting )
MIG 15-25-527, Road Number 1, Phase I & II, KPHB Colony, Kukatpally, Medchal District Landmark: Hyderabad and Warangal Near GHMC Ground 9381285354
Copyright © 2020 Cosmetic Plastic Surgery Centre. All Rights Reserved.
Symptoms of black fungal disease
Mucormycosis can often have warning signs that are very similar to normal sinusitis. Because of this, Sahu says people in the risk category, and especially those recovering from Covid-19, should be careful not to:
Rhino-orbital-cerebral mucormycosis (of the nose, eyes, and skull): congestion or obstruction of the nose; blackish or bloody nasal discharge; Facial pain, numbness, or swelling; Headache or pain in the eyes and orbit; Toothache, sagging tooth or jaw damage; blurred or double vision with pain; Tingling in the face; Fever and blackish skin lesions.
Inflammation of the lungs (affects the chest): fever, cough, chest pain, blood in the sputum after coughing, worsening of respiratory problems.
Doctors recommend that patients with any of these symptoms should see a doctor right away, because mucormycosis is an aggressive infection and can spread quickly throughout the body.
Where to see a doctor
Sahu recommends that aggressive black fungus infection requires an aggressive medical approach. A general practitioner may not be enough for this. “In such cases, a multidisciplinary approach is required. These can be specialists such as a neurosurgeon, an ENT surgeon, a cardiovascular surgeon, and an oral and maxillofacial surgeon, and specialists such as an infectious disease doctor, ”she said.
She adds that cases of mucormycosis can occur as early as eight to ten days after the detection of Covid-19, up to 60 days afterwards. The two to six week period after Covid-19 is detected is the most important, Sahu adds.
If even a single symptom occurs, patients should consider it a medical emergency.
How is mucormycosis treated?
“All cases of mucormycosis should be treated as a medical and surgical emergency,” says Sahu. Sometimes surgery may be needed to remove the diseased tissue and stop it from spreading. In some cases, antifungal drugs must also be given intravenously to patients, which can result in hospitalization.
These oral or injection drug treatments usually last six weeks and can last up to six months. In India, each of these antifungal injections can cost around Rs 7,000 (about $ 100), and it takes a patient up to nine per day. A course of at least three weeks can cost up to Rs13 lakh or more than ten times the median annual salary in India.